As the global monkeypox outbreak grows, so too, it seems, has confusion about the virus, how it spreads and who is currently at high risk for becoming infected. There is also public anxiety due to the uncertainty surrounding the current disease transmission dynamics.
On 23 July 2022, the World Health Organization declared monkeypox a Public Health Emergency of International Concern.
On 3 June 2022, WHO convened a group of experts who underlined the need for expedited studies to better understand the disease epidemiology, its clinical consequences, and the role of various modes of transmission. Experts also emphasized the need for clinical studies of vaccines and therapeutics to better document their efficacy and understand how to use them in this and future monkeypox outbreaks.
But we’re not starting from scratch unlike with COVID-19. Monkeypox is not a new disease and the monkeypox virus is not a novel one.
Number of confirmed, probable, and/or possible monkeypox cases between 2010–2019
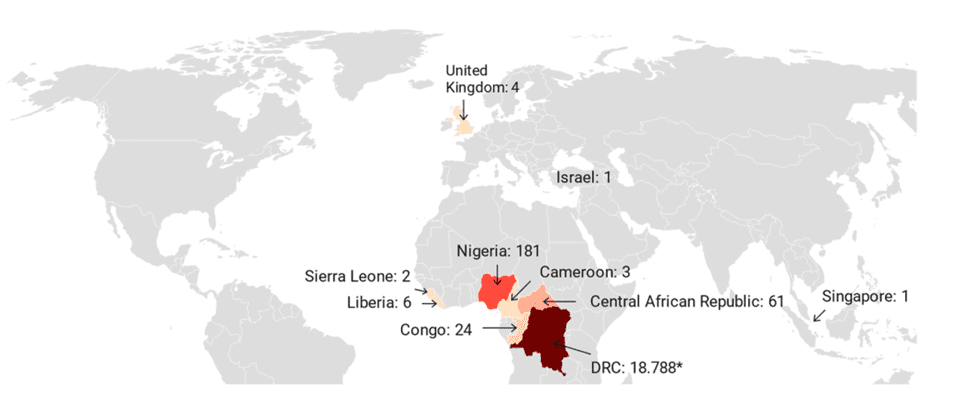
Monkeypox was not reported outside Africa until 2003, when an outbreak of 47 confirmed or probable cases occurred in the US following exposure to infected pet prairie dogs, which had acquired the monkeypox virus from infected animals imported from Ghana.
The most number of articles was published in a year when monkeypox was reported outside of the African continent in 2003. In the past decades, we have seen a similar reluctance to research and control some other pathogens with epidemic potential (Zika and Ebola as recent examples) which were largely reported by low- and middle-income countries.
Before the 2022 global outbreak, almost all monkeypox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs. There have been several travel-associated cases of monkeypox, all following exposures in Nigeria. There was one case in Israel in 2018, three in the UK – two in 2018; one in 2019 –and one in Singapore in 2019. A fourth case in the UK was the result of a healthcare worker getting infected with the virus in a hospital.
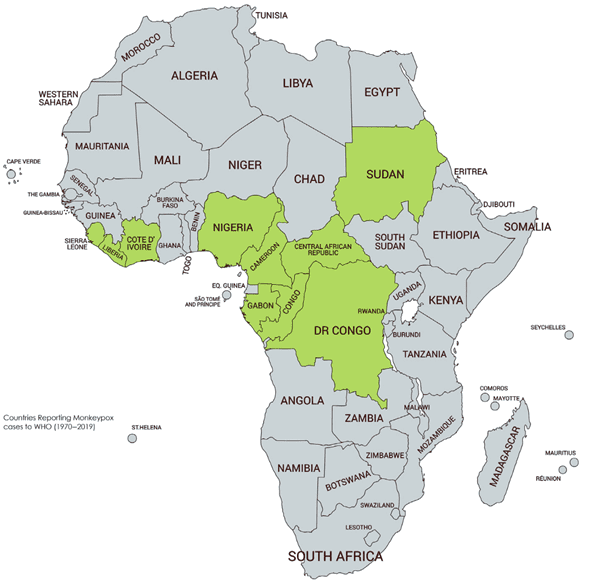
Since it was first diagnosed in 1970 in the Democratic Republic of the Congo, human monkeypox has appeared in 10 African countries. Examples include Nigeria, where the disease re-emerged in the last decade after a 40-year hiatus. In 2022, an outbreak of cases began occurring in multiple countries where monkeypox had not normally been present, including in the United States.
Human-animal interaction
https://www.binasss.sa.cr/mono/8.pdf
Monkeypox , according to the World Health Organization, has historically been reported from: Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Ghana (identified in animals only), Ivory Coast, Liberia, Nigeria, the Republic of the Congo, Sierra Leone, and South Sudan.
Monkeypox can infect a wide range of mammalian species, but scientists are yet to exactly pinpoint its reservoir – though there is evidence that squirrels and other types of rodents can naturally harbour the virus. The virus has only been isolated twice from a wild animal, a rope squirrel in the Democratic Republic of Congo and a sooty mangabey in Ivory Coast.
Human monkeypox cases in occur when there is an interaction with these infected animals. The majority of them arise from zoonotic spillover – with the virus crossing over from an animal to a human, when humans invade jungles and forests, the natural environment of the animal reservoir. There is money to be made in trapping wild animals and selling them as bush meat in local markets. Civil wars, refugee displacement, farming, deforestation, climate change, demographic changes, and population movement may have led to a spread of monkeypox-infected animals and increased their interaction with humans across West and Central Africa. According to WHO, overall cases of monkeypox in endemic countries in Africa have been rising since 2017, except in 2021 where there was a sudden drop.
Unfortunately, monkeypox outbreaks in Africa are rarely reported, leading to an incomplete picture of the disease’s importance and to inadequate attention to prevent epidemic spread. This left many questions about the virus unanswered.
As of 24 August 2022, WHO’s key epidemiological findings indicate the outbreak continues to affect young people of male gender, with more than 98 % of cases being males with an average age of 36 years. Among cases with sexual orientation reported, almost 96% identified as men who have sex with men. Of all reported types of transmission, a sexual encounter was reported most commonly with more than 80 % of all reported transmission events.
What’s clear from the epidemiological evidence so far is that the current monkeypox epidemic is being driven overwhelmingly by close intimate contact between sexual partners. What’s less clear is whether urine, feces, blood, semen, or vaginal fluids can spread the virus, the extent to which people without symptoms can infect others, and how much of a role inhaled respiratory particles are playing in transmission.
Monkeypox’s spread in non-endemic countries has led many to wonder if, like SARS-CoV-2, the virus has mutated to allow for easier human-to-human transmission. Monkeypox is a type of DNA virus, which detects and repairs mutations better than RNA viruses like SARS-CoV-2, and thus is less likely to quickly acquire mutations that promote its spread.
However, new research suggests the monkeypox virus has acquired an average of 50 new mutations compared to strains detected from 2018-2019. This is roughly 6 to 12 times more than the expected 1-2 mutations per year. Researchers think this “accelerated evolution” could potentially be linked to the virus adapting to evade the host’s immune response to fight infection.
Scientists are also worried that sustained transmission of monkeypox worldwide could see the virus begin to move into high-risk groups, like pregnant women, immunocompromised people and children.
Children can catch monkeypox if they have close contact with someone who has symptoms. Data from previously affected countries show that children are typically more prone to severe disease than adolescents and adults. There have been a small number of children with monkeypox in the current outbreak. Compared with healthy adults, complications are more frequent in children with an increased risk of secondary bacterial infections, sepsis, respiratory complications due to pharyngeal abscess and pneumonia, or encephalitis.
Although information regarding the effects of monkeypox infection in pregnant women is scarce, transmission of monkeypox has been associated with fetal death and congenital infection. Congenital infections affect the unborn fetus or newborn infant. They are generally caused by viruses that may be picked up by the baby at any time during the pregnancy up through the time of delivery.
Monkeypox is expected to be more severe in pregnant women than in healthy individuals who are not pregnant, particularly during their third trimester.
Of the two vaccines being used in the United States to prevent monkeypox— named Acam2000 and Jynneos—only the latter could be considered safe for pregnant people, though human data is limited. According to the US Centers for Disease Control, Acam2000 is not recommended due to the risk of pregnancy loss, congenital defects, and other adverse effects.
Both the US Centers for Disease Control and the WHO estimate that the available Jynneos smallpox vaccine (also known as Imvamune or Imvanex) is about 85% effective against monkeypox. The Jynneos vaccine is an attenuated (weakened) live virus vaccine approved by the US Food and Drug Administration in 2019 for individuals at high risk for smallpox or monkeypox infection.
The use of the vaccine is based on an observational study involving 245 people infected with monkeypox in Zaire (now the Democratic Republic of the Congo) between 1981 and 1986, and more than 2,000 of their contacts. Individuals who had a visible scar from a jab with the first-generation smallpox vaccine were about seven times less likely to contract monkeypox after exposure to an infected person than those who were unvaccinated.
The cessation of smallpox vaccination in 1980
The emergence of human monkeypox cases in Africa can also be attributed to the global end of smallpox vaccination in 1980.
On 8 May 1980, WHO declared the world free of smallpox and this led to a cessation of the use of vaccines against the smallpox virus. It is well documented that the smallpox vaccination does not just protect against smallpox but also protects against several other pox viruses. Data suggests that the smallpox vaccine is about 85% effective against clinical monkeypox virus infection.
In 2010, clinicians started seeing a major increase in human monkeypox incidents in DRC 30 years after smallpox vaccination campaigns ended. In 2010, only 24.5% of the DRC population had evidence of a smallpox vaccination scar and more than 90% of monkeypox cases identified were born after mass smallpox vaccination campaigns officially ceased.
Data from DRC suggest that vaccine-induced immunity is long lasting because individuals who were vaccinated against smallpox over 25 years ago still appear to be at significantly reduced risk of monkeypox. The average age in the DRC is about 18 and a half years old, and this means that an overwhelming majority of the population does not have immunity against all the pox viruses.
However, scientists are cautious and point out that the highly cited figure should not be taken at face value, particularly in the context of the current outbreak. The World Health Organization has revealed there have been a number of breakthrough cases of monkeypox after preliminary reports detail the efficacy of the vaccine.
At a media briefing on 22 August 2022, Dr Rosamund Lewis, WHO’s technical lead for monkeypox, discussed reports of breakthrough monkeypox cases in people who received a prophylaxis vaccine following exposure to the virus.
“What we’re seeing are breakthrough cases, which are not really surprises, but it reminds us that a vaccine is not a silver bullet, that every person who feels that they are a risk, and appreciates their own level of risk, and wishes to lower their own level of risk have many interventions at their disposal, which includes vaccination where available but also protection from activities where they may be at risk,” Lewis said.
Another pressing problem is that the Jynneos vaccine, manufactured by Bavarian Nordic, is in short supply. The catch is that Denmark-based Bavarian Nordic is the sole manufacturer of the Jynneos vaccine and analysts are sceptical that the company can produce enough supplies to match up against the likely worldwide need.
Fractional dosing to offset vaccine shortage
To offset the shortage of monkeypox vaccine, several countries, including the United States, Britain and Spain, are stretching out the available supply by offering eligible patients smaller but equally effective doses of the vaccine.
The safe and clinically-approved approach, known as ‘fractional dosing’, has been commonly used in other worldwide outbreaks when vaccine supplies are constrained. Fractional dosing could maximise the number of doses that can be administered without compromising protection, with clinical study results showing it provides a near-identical immune response in patients.
Under the approach, eligible people aged 18 and over will be offered a 0.1ml dose of the smallpox Jynneos vaccine, instead of the 0.5ml dose that is typically administered. This will potentially enable up to a 5-fold increase in the number of people that can be offered vaccination.
In the United States, public health officials are considering dose-sparing approaches, e.g., using one dose of Jynneos administered subcutaneously instead of the licensed two doses and/or using two doses administered at a fraction of the standard dose by the intradermal route of administration of the attenuated vaccine. However, a complicating factor is the requirement for health workers to get extra training for the delicate intradermal procedure to inject subcutaneously.
According to a Reuters tally of government statements there are just 1.5 million vials of Bavarian Nordic’s monkeypox vaccine either administered or currently available in the 10 worst-affected countries, which account for nearly 90% of all cases – and most of the doses have been allocated to the United States. The WHO estimates that between five million and 10 million doses of vaccine will be needed to protect all high-risk groups, with a current focus on certain men who have sex with men and contacts of people infected.
Another COVID rerun: Africa coming in last
In the current COVID-19 pandemic, Africa has struggled to get vaccines. At one period, more than 80% of people in Africa had not yet received a single dose. The issue of vaccine supply and access is at the heart of the difficulties in trying to increase vaccination rates in Africa.
With monkeypox, we’re now seeing a COVID redux on the continent. Africa, the only continent where monkeypox is endemic, has yet to receive vaccines for the virus as the infectious disease spreads around the world.
The Africa CDC is in talks with developers to get shots “as soon as possible” for both monkeypox and smallpox. Vaccines for the latter disease, which has been eradicated, can also be used against monkeypox.
Still, Africa is dealing with at least six significant disease outbreaks aside from COVID-19 and monkeypox, including the Marburg virus, Lassa fever, cholera, measles and wild polio, putting strain on often limited resources. For this reason WHO is not stressing vaccination as the main strategy for controlling the monkeypox outbreak, focusing instead on surveillance and contact tracing.
References
Other useful resources from Internews: