This is how we prepare for the next public health crisis.
by Beatrice M. Spadacini
Every disease outbreak is an opportunity to reflect on what we have learned from past public health emergencies and what we can do better in the future. Two plus years into the COVID-19 pandemic and one thing is for sure: ramping up resources during a panicked response to a disease outbreak and then receding into neglect mode once the disease is under control, is not a sustainable approach. This leaves the world more vulnerable to future health threats and less resilient to bounce back quicker and stronger.
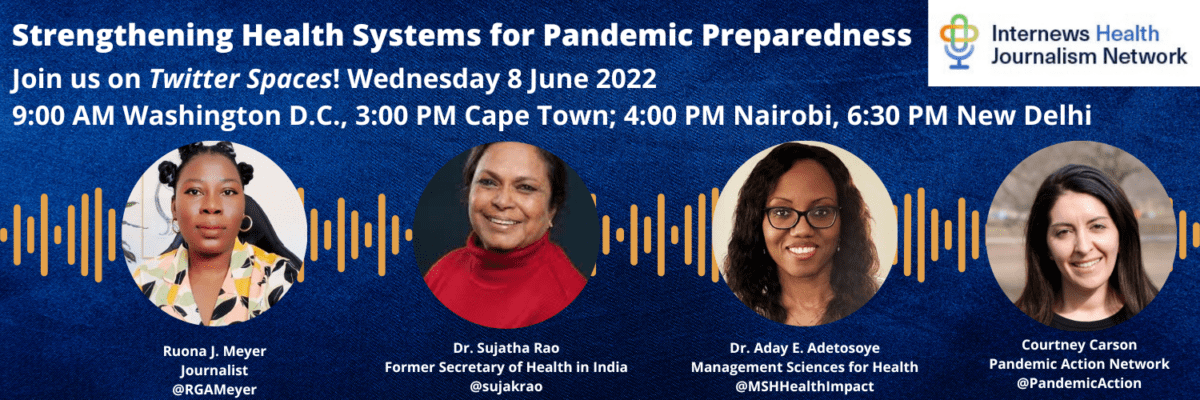
So, what can journalists do to ensure that everyone is better prepared to handle the next public health emergency? How can we keep people woke, so to speak? This is what we asked on June 8 to a panel of health experts in our second Twitter Spaces event of the year dedicated to Reporting on Health System Strengthening and Pandemic Preparedness.
Investigative reporter Ruona Meyer, who moderated this session, kicked off the discussion by acknowledging that the term “health system strengthening” is not media friendly and that it must be “unpacked.” Dr. Aday E. Adetosoye, Vice President of global health programs at Management Sciences for Health (MSH), represents an organization that supports governments in building strong health systems and achieving universal health coverage. She offered a tangible explanation of this goal.
“It is a system that has the resources to provide high-quality services when responding to a disease outbreak and can quickly mitigate the spread of disease. It must be able to initiate a timely and coordinated response with a competent and well-trained workforce. It has a surveillance system that tracks and quickly communicates data from identification and diagnosis of the disease to the treatment and control of it. This includes data on deaths and mortality rates,” said Dr. Adetosoye.
As COVID-19 clearly demonstrated however, leadership cannot be underestimated. Dr. Adetosoye added,
“I want to be clear. A strong and resilient health system does not only feature the essentials of a primary health care system and a functioning public health infrastructure. It also requires effective leadership, public trust, and the political will to move quickly and differently.”
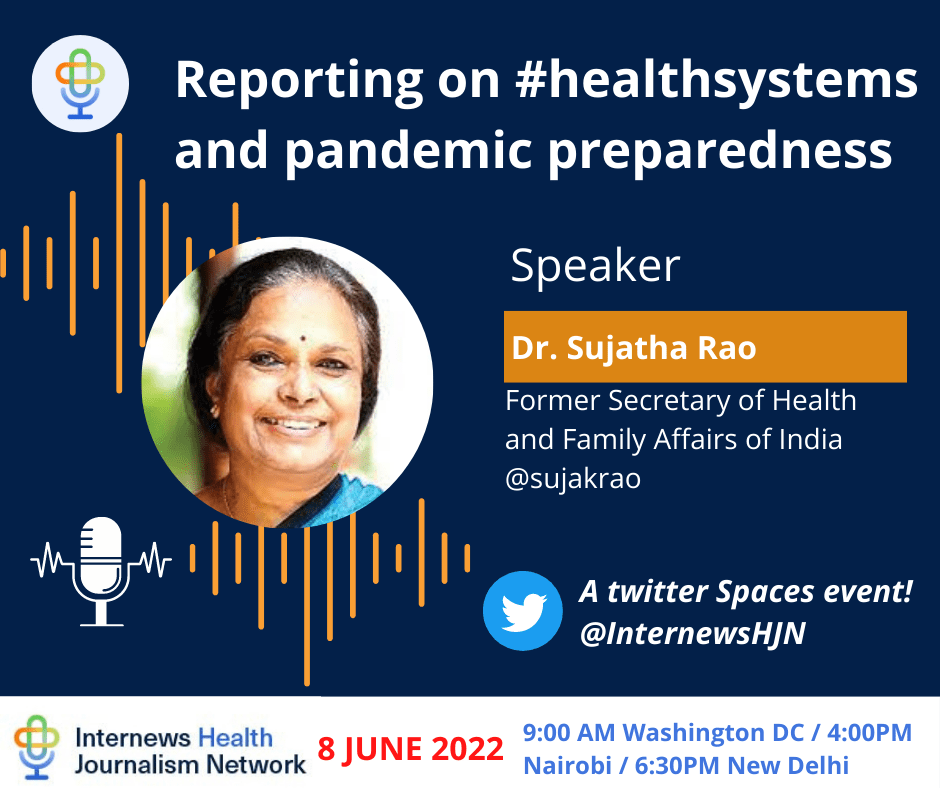
Dr. Sujatha Rao, former Secretary of Health and Family Welfare of India, spoke about the devastating impact of the Delta wave in her country and how it tested their capacity to manage it. “The only way to cope is to decentralize pandemic management,” said Dr. Rao. “We must embrace the lessons we learned during the 2014 Ebola crisis in West Africa. It is only when the primary health care system can take care of patients that we can cope. Rushing all patients to hospitals during COVID-19 revealed the infrastructure gaps of our health system in India. We simply did not have enough oxygen supply for everyone. We did not expect to be hit so hard. At one point we had 50,000 cases per day in Delhi.”
Dr. Rao emphasized that COVID data does not consider the collateral effects the pandemic had on other illnesses, on children’s mental health and the rise in domestic violence cases during lockdowns. Furthermore, maternal mortality rates in India went up 30 percent and TB infections rose by 40 percent. When talking about preparedness, Dr. Rao raised an important question, “Can we mortgage an entire health system to one infection?” Adding that it has taken us over two years and we still have not reached the epidemic stage of this virus, she said “I think we need to redesign our health systems today, keeping in mind that COVID-19 is still out there, and that we must learn to live with it. A strong health system is people-centered and is anchored in the community.”
Courtney Carson, Senior Program Officer with the Pandemic Action Network, recognized the critical role of community engagement and leadership in both health system strengthening and pandemic preparedness. She too acknowledged the broad ripple effects of COVID-19 and highlighted the need to leverage these as an imperative to invest in pandemic preparedness. Carson added that,
“It is clear that strong health systems underpin global health security and pandemic preparedness. However, some investments are specific to pandemic preparedness. Supporting epidemiologists and addressing the human-animal interface and disease spillovers is necessary. If we only apply a preparedness lens to health system strengthening, we may miss critical pieces. We need both, and one is not sufficient without the other. We need investments in building strong health systems and investments in specific preparedness capacities.”
Carson underscored that preparedness is rooted in the memory of previous public health crisis. For the first year, “COVID was a [disease]without approved vaccines or treatments. There was a shortage of masks and PPEs [Personal Protective Equipment] while hospitals everywhere were overflowing and overburdened. These are real examples we have all lived through where something was missing because the preparedness system was broken. As communicators, we need to tap into these lived experiences and drive action and change while COVID-19 is still real and tangible. If we wait too long, we will forget and fall victim again to the cycle of panic and neglect.”
All speakers acknowledged that the media is critical in mounting an effective response to a disease outbreak however, how authorities manage external messaging must be improved. Kenyan journalist and HJN member Eunice Kilonzo-Muraya asked how countries can aspire to create strong health systems without leaving anyone behind in the process. “The key word is equitable,” said Dr. Adetosoye of MSH. “When you look at country budgets, you will notice that defense budgets are often much higher than health budgets. This is something we all need to investigate. To build strong and resilient health systems that provide quality services to all citizens, countries must shift how they allocate their resources. Quality health care must be available to all on a regular basis, not just in the face of a pandemic.”
You can listen to the full recording of the June 8 Spaces here.