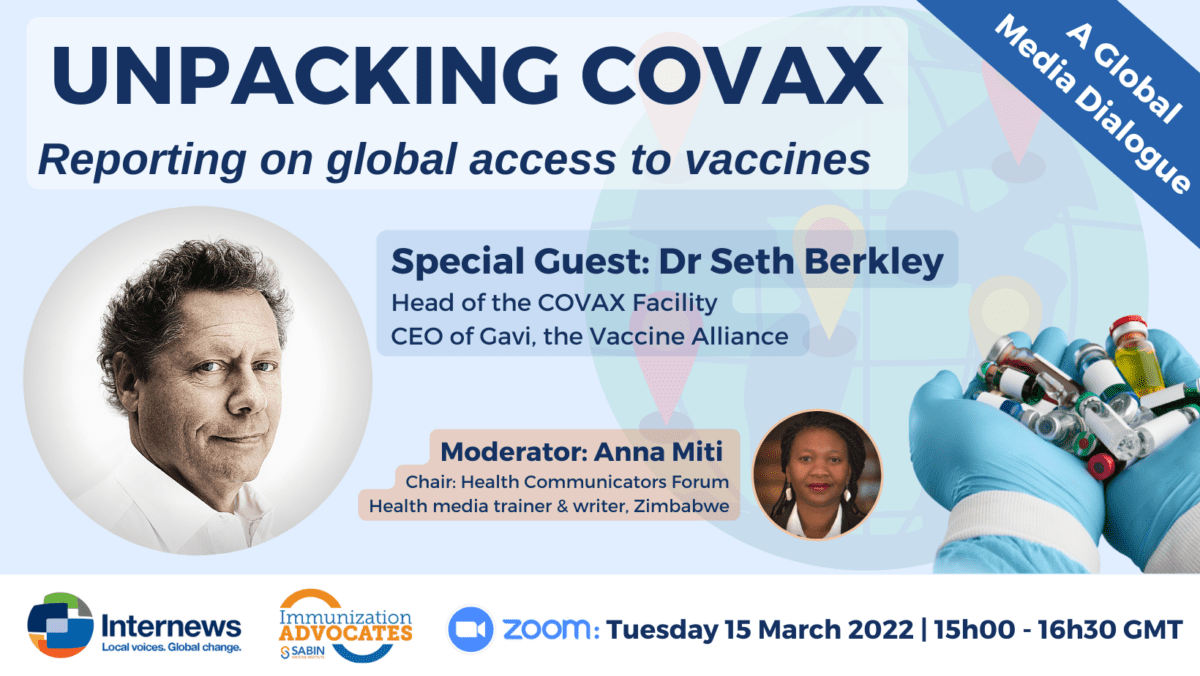
On 15 March 2022, Internews in partnership with the Sabin Vaccine Institute hosted Dr Seth Berkley, CEO of Gavi and Head of COVAX, for an informative webinar titled “Unpacking COVAX: Reporting on Global Access to Vaccines.” Moderated by broadcast journalist from Zimbabwe, Anna Miti, the session saw well over 100 participants from all over the world, particularly LMICs, who brought forth important questions about COVAX.
What is COVAX?
To provide some background, Berkley highlights that COVAX was created within the first week after reports of COVID-19 came out of Wuhan, China. The idea for COVAX was inspired by the 2009 H1N1 pandemic, he says, where wealthy countries bought up almost the whole of the global vaccine stock. COVAX is a global mechanism for equitable access to vaccines, especially for vulnerable countries, states Berkley.
The first COVAX vaccines were delivered in lower income countries 39 days after wealthy countries got them, nothing like this has ever happened before, he continues. “Now, there’s enough global supply and demand that COVAX can provide countries with what they need as well as guidance on vaccine rollout.”
We plan for the worst and hope for the best, he says.
Currently, Berkley states that COVAX is working on supporting the delivery of vaccines in countries with low absorption rates, or in other words the rate at which vaccines make their way into the upper arms (or buttocks) of a given population.
“People are saying we’re done with the virus, but the virus isn’t necessarily done with us. We continue to accelerate the vaccine efforts. It is absolutely critical that high risk populations in every country in the world are vaccinated,” urges Berkley.
What about the challenges to vaccine acceptance?
Berkley states that it’s not an issue exclusive to the developing world.
“Statistically the country that has the highest vaccine hesitancy is France, home of Louis Pasteur. The lowest vaccine hesitancy is in Rwanda, and what’s interesting is [that] mostly people in countries know about these diseases and want to protect their families, so it’s easier to educate. This particular [COVID-19] vaccine has become politicised globally, and there’s all kinds of crazy rumours. We have a bigger problem with concerns about this vaccine than we’ve had with any other vaccine I’ve worked with and that is a real challenge.”
What factors determine priority for distribution of COVAX vaccines?
The WHO has put together an equitable allocation mechanism including an independent review group to look at it to make sure that it’s fairly done if there is a shortage of supply, says Berkley. “As of today, there is no shortage of supply so we can meet the needs of countries within some reason, as they request doses, so then it’s an issue of the country communicating well what their priorities are.”
What’s being done to ensure Western countries share excess vaccines?
“We want to make sure that the donations have the [appropriate] shelf life and are the vaccines that people want. We don’t control that completely, sometimes we offer a vaccine to a country and the country says they don’t want that vaccine. [We are] trying to have it be a coordinated process but there’s a lot of issues around vaccine diplomacy, we can’t control that,” says Berkley.
Question from Dr Jaya Shreedhar, Internews Pandemic Media Mentor, medical doctor (India): What did India do right?
When we started COVAX, India was a priority, says Berkley. “Initially, India started vaccinating early and Indian manufacturers produced a lot of doses. What India did that helped India was it stopped all exports, but that also hurt India. India is one of the major suppliers to the world, and what happened is that countries received some doses early and that was part of the system. When that stopped, all [of] those doses went to India.”
Comment from Adele Baleta, Internews Pandemic Media Mentor and health/science journalist (South Africa):
“Some are saying that COVAX was designed primarily with the global north groups in mind, and notably absent were the critical perspectives of regional bodies such as the African Centres for Disease Control and Prevention, and really any meaningful representation from LMICs, and some are saying that, that maybe would have been a better way to go about it, to structure COVAX differently which might have avoided the challenges we are facing now.”
“GAVI has representation from 56 low income countries, so those countries were represented from the beginning,” responds Berkley. “The AMC is larger, it’s 92 countries, so we created a series of bodies where we could have discussions. The challenge in this is, at the end of the day, health is a national function and so we work closely with the AU or the EU, at the end of the day, a decision on a certain vaccine is a country’s decision. What we had to do was make sure every country chose what vaccines they wanted and do the work on the indemnification and liability, and that made it very complicated. What would make a difference in the future is if we can create regional bodies that can cut across those issues. We don’t have those so it literally requires a country by country discussion.”
Will COVAX exist after this pandemic?
“My own belief, if COVID-19 vaccines are required, we are likely to fold that into routine vaccines. We want to get out of emergency mode and it would be like [providing] countries with [any] other vaccines. We would try to [make it routine]. Whether COVAX would exist or not is still being discussed,” informs Berkley.
Question from Esther Nakkazi, media trainer, science and technology journalist (Uganda): Would COVAX buy vaccines from local African manufacturers, this is a concern that Africa has?
“We welcome more manufacturing of vaccines on the African continent, and we would be delighted to purchase those vaccines,” says Berkley. There’s a couple of caveats here, he says, first of all, our long term goal is supply security, so what we will do is pay for different manufacturers including some that might be more expensive. He adds that they have to be WHO pre-qualified and meet global standards, so one of the questions now will be which vaccines will these new manufacturers make. There are already a lot of COVID-19 vaccines so there might be an eventual over supply which means other vaccines should be manufactured, states Berkley.
Question from Graziella Almendral, Internews Pandemic Media Mentor, journalist (Spain):
In 2021, LAC was one of the top regions globally for reported COVID-19 deaths, [and] vaccines weren’t arriving in early 2021. This situation created political tensions and vaccine hesitancy as many people did not understand why they weren’t receiving vaccines. Is COVAX assessing epidemiological scenarios in addition to equity factors when programming vaccine deliveries as some governments requested?
“PAHO, unlike other WHO regions, is different,“ says Berkley. “We work with Unicef to deliver vaccines in other regions but we work with PAHO in LAC. Our goal ultimately is to serve every country and get them the doses they need.” Berkley explains that in LAC, many of countries are higher income countries and do not form part of the advanced market commitment, don’t have the donor funds, and therefore in our discussions with them, they are so-called self-financing participants meaning they can buy doses through COVAX if they want but they can also buy doses bilaterally.